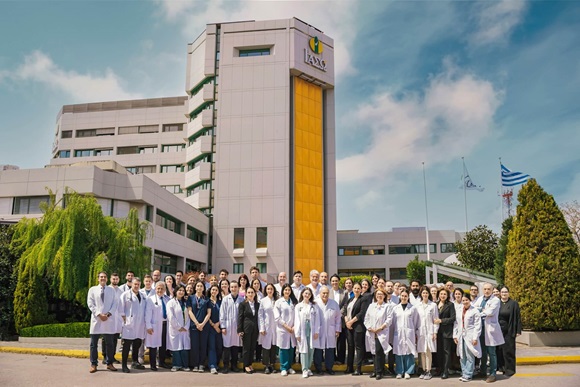
Support Departments
European as well as International standards and guidelines regarding all areas of responsibility of the departments of Central Sterilization have been established in an effort to ensure the sterility of materials and provide traceability at every stage.
Sterilization must be performed according to a validated and certified method. Relevant data are archived and available at all times.
The Central Sterilization Unit at IASO is responsible for the sterilization of the surgical tools- materials used by the various Treatment Departments, and their maintenance, selection, packaging and storage, along with the distribution of sterile items to the operating rooms and other departments.
In addition to surgical tools, the Sterilization Unit also processes every single item that comes in contact with the patient and must also be sterile (clothing, surgical table equipment, gauzes, etc.).
Organization and Operation of the Central Sterilization Unit
The Clinic’s sterilization methods are
- Automatic steam furnaces (Pre vacuum EN 285)
- Formaldehyde furnace
- Plasma furnace (Hydrogen peroxide furnace)
Quality Control
Furnace Control (ΕΝ 867-4)
The steam furnaces are daily tested to ensure that the air has been adequately removed and that steam penetration is sufficient.
This testing is performed using the BOWIE - DICK test of steam penetration in an empty furnace and the result of the test indicates whether sterilization is possible.
Exposure Control (ΕΝ 867-1 κ´2)
The exposure test is a way to distinguish between sterilized and non-sterilized materials at a glance.
It includes the use of an indicator strip which is externally affixed on the packaging and changes color following steaming in the furnace. It verifies that the package and the material it contains have undergone the sterilization procedure.
Load Testing (EN 867-1)
Testing of each sterilized load is performed using a biological and chemical indicator. The biological indicator contains an enzyme of Geobacillus stearothermophillus that relates to the growth of the spores, and evidences that the sterilized load is free of bacteria and, therefore, suitable for use.
Details relating to the biological indicator are filed in the "Steam-Formaldehyde Load Record" form and in the "Plasma Load Record" form. The chemical indicator of the load promptly indicates the achievement of appropriate load sterilization and is used with a simulation device (PCD).
Package Control
Testing of each sterilized package is performed using chemical indicators. The chemical indicator is placed within each package, tray and container, and evaluates whether the means of sterilization have penetrated inside, confirming that it has been exposed to the proper sterilization conditions.
The chemical indicator bears a color indication which changes following the sterilization procedure according to the manufacturer's specifications. The evaluation of the chemical indicator is performed by the user. The chemical indicator is attached to the medical records of the patient as a proof of the use of sterilized medical tools.
Record Maintenance
The final stage of a successful sterilization procedure is record maintenance. Record maintenance consists of the following:
- Bowie -Dick Test filing
- Filing of sterilization cycles on the furnace charts.
- Filing of the biological indicator in the «Steam-Formaldehyde Load Record» form and «Plasma Load Record» form.
- Filing of the chemical indicator in the patient's medical records.
Record maintenance facilitates the easy detection of the sterilized material (traceability).